

ICD-10 (International Classification of Diseases) is the diagnostic coding system implemented by the World Health Organization (WHO). ICD is mainly used for epidemiological tracking of illness and injuries.
The ICD-10 code set has more specific codes for illness and injuries and clinical information that are in line with today’s healthcare practice. ICD-10 has two sets of codes: ICD-10-CM (Clinical Modification) and ICD-10-PCS (Procedure Coding System)
How is ICD-10 different from ICD-9?
The ICD-10-CM codes are entirely different from the ICD-9-CM codes. The ICD-10 codes have fundamental changes in the structure and the concepts. ICD-9 codes do not convey specific information in the codes.
For instance, if a patient reports a cut on his/her left hand, the ICD-9 codes do not differentiate whether the wound is in the left/right hand. Later, if the patient is again diagnosed for a cut in the right hand, the same ICD-9 diagnosis code would be repeated. ICD-10 codes identify this difference of right and left, encounter information, and other vital clinical information.

Example
S52.521A – Torus fracture of lower end of right radius, initial encounter for closed fracture
In this example, first three characters (S52) is the “Category”, fourth and fifth characters (‘5’ & ‘2’) represent the clinical detail and anatomic site, sixth character (‘1’) indicates the right or left side, and the seventh character (‘A’) provides the additional information such as type of encounter and so on.
Comparison of ICD-9 and ICD-10 Diagnosis Code Sets
|
ICD-9 |
ICD-10 |
|
Approx. 13000 codes |
Approx. 68000 available codes |
|
3–5 characters in length |
3–7 characters in length |
|
Lack of specificity of detail |
Specific detail |
|
Lack of identifying right/left (i.e.) laterality |
Able to identify laterality |
|
First digit may be Alpha or numeric; 2–5 are numeric |
1st digit is Alpha; 2nd and 3rd digits are numeric; 4–7 are either alpha or numeric |
|
No placeholders to fill empty positions |
A place holder ‘X’ is used to fill empty character positions (4, 5, and 6th positions) |
Why move from ICD-9 codes to ICD-10 codes?
ICD-9 codes were developed almost 30 years ago. These codes are now obsolete and outdated, and lack the specificity of diagnosis information required for the current healthcare practice. The current structure of ICD-9 codes limit the addition of new codes as well as most of the ICD-9 categories are full, thereby limiting space to add new codes.
Why ICD-10 is better than ICD-9?
ICD-10 has five times more number of diagnosis codes as well as categories that allow a specific way of representing the medical diagnosis and procedures.
What is the impact created by ICD-10 codes?
If the ICD-10 codes are implemented correctly, the specific codes corresponding to the patient problem will improve the claim settlement process. This will ensure error free claims to the patients.
ICD-10 codes have to be implemented by all the healthcare vendors, payers, providers, regulatory agencies and others who currently utilize the ICD-9 codes.
Does ICD-10 coding impact the CPT codes?
No. The ICD-10 codes will not affect the Current Procedural Terminology (CPT) codes used for outpatient procedures. The ICD-10 codes are applicable for hospital inpatient procedures.
ICD-10-PCS (Procedure Coding System), designed by 3M Health Information Management for Centers of Medicare and Medicaid, is the code set to replace the Volume 3 of ICD-9-CM for inpatient procedure reporting. This ICD-10-PCS has approx. 71000 alpha-numeric codes which has seven digits.
Structure of ICD-10-PCS Codes:
In the structure,
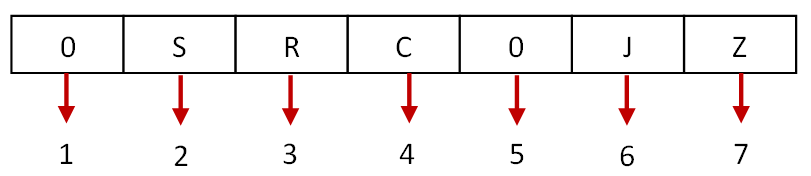
For the example shown above, ICD-10 code for knee joint replacement (0SRC0JZ – Replacement of Right Knee Joint with Synthetic Substitute, Open Approach) means the following:
For more information on ICD-10-PCD codes, click here: https://www.cms.hhs.gov/ICD9ProviderDiagnosticCodes/08_ICD10.asp
What are the benefits of ICD-10?
Moving to ICD-10 will speed up the medical reimbursement process in the industry and reduce the payment errors. It also enhances the quality of healthcare offered to patients.
What is the timeline to move from ICD-9 to ICD-10?
The Department of Health & Human Services (HHS) published the final rules for adoption of new HIPAA standards on January 16, 2009. The rule mandates the replacement of ICD-9-CM code sets with ICD-10-CM and ICD-10-PCS code sets by October 2013. However, on April 17, 2012, the Department of Health & Human Services has published a proposed rule that will delay the compliance date for ICD-10 from October 1, 2013 to October 1, 2014.
What is the non-compliance penalty?
The HHS has also enforced laws and penalties for non-compliance of ICD-10. Organizations will be subject to a fine of $1 per covered life per day for non-compliance with the certification requirements. The penalty shall double if the organization provides incomplete or inaccurate information for compliance.
Where can I get my copy of ICD-10 codes online?
You can find the ICD-10-CM and ICD-10-PCS code sets on the CMS website
ICD-10-CM Diagnosis Code Sets -
https://www.cms.gov/ICD10/11b14_2012_ICD10CM_and_GEMs.asp
ICD-10-PCS Code Sets -
https://www.cms.gov/ICD10/11b15_2012_ICD10PCS.asp
What should I do to get started?
The first step towards ICD-10 compliance is to carry out an “ICD-10 Assessment, Impact Analysis, and Planning”. ViSolve Healthcare IT can help you plan and assist you throughout the process for achieving the ICD-10 Compliance. Contact our consultants today at +1-(408) 850 2243 or write to us at [email protected].
What is the difference between EMR and EHR?
EMR and EHR are two terms that are used quite interchangeably these days. Several definitions exist for both and there have been heated discussions on forums about this.
So is there really a difference between the both that is worth knowing? Yes and here is the difference:
What is an EMR?What is the difference between unidirectional and bidirectional integration with a lab?
In a physician practice or in a hospital, the EMR/EHR needs to be integrated with the Laboratory to send the lab requests and receive lab responses electronically.
If only any one of the interface [lab request or lab response] is integrated, it is called as unidirectional integration.
Whereas in Bi-directional integration, both HL7 lab requests and HL7 lab responses are integrated electronically with the EHR
These are the two main models for patient consent to exchange personal health information through the HIE network.
Opt-in: Requires authorization from the patient through signing a standardized consent form, before the patient's health information may be exchanged through the network.
Opt-out: The patient is given notice – through mail, brochures and other means - and patient's health information will be exchanged through the network unless and until the patient formally raises any concern.
ONC- Authorized Testing and Certification bodies has been authorized by ONC under temporary certification program to perform testing on EHR modules / Complete EHR and can certify any EHR which meets the requirements.
What is the difference between modular certified EHR and complete EHR?
Modular certified EHR doesn't need to satisfy all the stage 1 meaningful use criteria. It is enough to get certified with security & privacy criteria plus few other criteria (of EHR vendor choice). Whereas complete EHR satisfies all the stage 1 meaningful use criteria.
I do use a modular certified EHR and I purchased some third party modules to meet some other criteria, do the third party modules also get certified?
Yes, if you are using any other third party softwares to achieve some of meaningful use objectives (like e-prescription), then it should also get certified.
Do ONC-ATCB certified products have to undergo re-certification for each new release?
For "minor product changes" [those modifications and updates to a certified product that are unlikely to affect the product's compliance with the certification criteria], retesting may not be required but the vendor is required to notify the ONC-ATCB and provide self-attestation that the changes are minor.
Modifications with a significant risk of affecting the product's compliance are considered to be a "significant product change". Retesting is required.
Is there any limit in number of CPT codes per bill?
Yes, CMS 1500 form accepts only six CPT codes for medical reimbursement from insurance payers.
Modifiers are two digit value used with CPT code has special consideration on payment. It may increase or reduce the amount of provider's reimbursement claims. CPT code provides the details about the services render to patient, modifier with CPT code are used to specify that service has been adjusted due to specified conditions.
Where the modifiers are shown in CMS 1500 and X12 forms?
In CMS 1500 form, modifier are used in field 24d for medical reimbursement. In X12, Loop 2400:SV101 is used to populate the modifiers informations.
In certain conditions, two or more modifiers are required to completely explain the services/procedures rendered to the patient by provider. Modifier 99 is used when two or more modifiers effects the billing. Modifier 99 is added to the basic procedure code and all other modifiers are listed in the 24d in CMS form.
If modifiers are allowed, what is the maximum number of modifiers can be used in CMS and X12 forms?
In CMS form, maximum number of modifiers allowed with each CPT code is four.X12 allows four modifiers separated with colon as delimiter.
Meaningful Use (MU) is a set of defined standards dictated by CMS (Centers for Medicare & Medicaid Services) led by the U.S. Government under the HITECH (Health IT for Economic and Clinical Health) to encourage healthcare providers to illustrate the use of certified Electronic Health Records on a ‘Meaningful Use’ basis, resulting in incentive payments in doing so.
MU improves the safety, quality, efficiency of patients/patient records and improves the care coordination, population and public health.
What happens if I do not get my EHR attested?
Not having to adhere to the said rules would result in incentives, in the form of payments, being revoked but also having being penalized for it in the end.If Medicare EPs do not demonstrate meaningful use of certified EHR by 2015, the Medicate payments will be reduced by 1% in 2015, 2% in 2016, and 3% in 2017.
Click here to know more about the incentives and penalties.
What is Medicare and Medicaid?
Due to the vast nature of medicine and practice available out there today, the CMS has divided the recipients of incentives into two categories of programs, thereby allowing proper care to the patient and rewarded accordingly.
Medicare is an insurance program run by CMS, an agency of the federal government. This program primarily serves patients over 65 years of age, young disabled and dialysis patients as well. The incentives for EPs (Eligible Professionals) under this category may go up to $44,000 if the MU certification is applied and followed upon.
Medicaid on the other hand, is an assistance program, led by local and state governments under federal governments, that serves patients who fall under the low income group of any age. If MU is applied and followed upon here, the incentives may be up to $63,750.
How many criterions should an EP/EH/CAH meet in order to be MU Stage 1 Certified?
In order to be MU Stage 1 Certified,
When will MU Stage 2 become effective?
The Stage 2 certification will be effective in the fiscal year 2014 for EHs and CAHs and in the calendar year 2014 for EPs.
How many criterions should an EP/EH/CAH meet in order to be MU Stage 2 Certified?
How much incentive can I receive under Medicare and Medicaid Incentive schemes?
In Medicare, EPs can receive incentives to a maximum of $44,000 over a period of five years (starting 2011 through 2015). In the first year of certification, the EP’s must demonstrate meaningful use of EHR system for a 90-day period. In the following years, they must demonstrate meaningful use of the EHR system for the full year.
In Medicaid, EPs can receive incentives to a maximum of $63,750 over a period of six years (starting 2011 through 2016). The providers will be eligible for incentives in the first year just by adopting, implementing, or upgrading the EHR technology. However, from the second year, providers must demonstrate meaningful use of EHR system to be eligible to receive incentive payments.
What are Clinical Quality Measures? Why are they important?
CQMs are tools that help to assess the treatment, observations, processes, and outcome of patient care in the healthcare facility. It assesses the degree to which the Health Care Provider (HCP) delivers the services and results appropriate to the patient in a particular timeframe (reporting period). Measuring the quality of patient care helps in identifying the areas of improvement in patient care.
Who are Eligible Professionals and Eligible Hospitals?
| EPs | EHs |
|
Doctor of Medicine (MD) Doctor of Osteopathy (DO) Doctor of Podiatric Medicine (DPM) Doctor of Chiropractic Doctor of Oral Surgery Doctor of Dental Medicine Doctor of Optometry |
Subsection (d) hospitals” in the 50 states or DC that are paid under the Inpatient Prospective Payment System (IPPS) Medicare Advantage (MA-Affiliated) Hospitals Critical Access Hospitals (CAHs) |
|
Physician Assistant (PA) Nurse Practitioner (NP) Clinical Nurse Specialist Certified Registered Nurse Anaesthetist Certified Nurse Midwife Clinical Psychologist Registered Dietician Clinical Social Worker |
Acute care hospitals with atleast 10% Medicaid patient volume Children’s hospitals |
|
Physical Therapist Qualified Speech-Language Therapist Occupational Therapist |
The movement of a patient from one setting of care (hospital, ambulatory primary care practice, ambulatory specialty care practice, long-term care, home health, rehabilitation facility) to another.The EP who transitions their patient to another setting of care or provider of care or refers their patient to another provider of care should provide summary care record for each transition of care or referral.
Can an Eligible Physician receive incentives from both Medicare and Medicaid?
EPs can receive incentives from both Medicare and Medicaid, but not in the same year. Even though the EP satisfies the requirements for both the incentive programs, they must choose only one (out of the two) program to be eligible to receive incentives.
However, once the payment is made, the EP has the option to switch between the two programs ONLY ONCE, BEFORE 2015.
Can all physicians in my facility/group be eligible for incentive payments?
Yes. As long as every EP meets the requirements and demonstrates meaningful use of the EHR, they will qualify for receiving incentive payments of $44000 over 5 years in Medicare and $63750 over 6 years in Medicaid.
How will I receive the incentive payments?
EHR incentives will be distributed to the Tax ID number (as a taxable income) provided by EPs when they register for Medicare and Medicaid program.
If an EHR is MU Stage 2 certified; can the physician use the same EHR to get attested for MU Stage 1?
YES. The physicians can use the EHR that is Stage 2 certified to get attested for Stage 1.
If an EHR vendor applies for complete certification, do they need to implement CQMImport and Calculate [170.314(c)(2)] feature?
NO. The EHR vendor need not implement the CQM Import and Calculate functionality if they are applying for complete certification. They can manually enter the CQM into the system.
However; this does not apply for vendors who do not apply for complete certification. In this case, they need to implement the CQM Import and Calculate functionality as a feature in the system.
What are the Gap Certification Features?
Gap Certification features are the set of requirements that do not have any change in Stage 2. The requirements remain the same as in Stage 1. The Gap Certification features are as follows:
If an EHR was certified by a certification body for Stage 1 and if they go to another certification body for Stage 2 Certification, would the gap certification features be the same as mentioned above?
YES. Gap certification remains the same across different certification bodies. So if you want to go to a different certification body for Stage 2 certification, you need not worry about gap certification features.